A lack of bowel control can be a very distressing symptom of MS causing discomfort and embarrassment. Bowel issues are often under reported and so it is unknown the exact numbers of people who suffer with bowel dysfunction. However, when reported symptoms can be managed and treated.
The bowel is the internal plumbing mechanism that takes the part of our food we can’t use in our bodies and makes it ready for disposal. The food we eat begins its journey at the mouth and proceeds down the oesophagus to the stomach. Major digestive action starts there and is continued in the small bowel or small intestine. The food, which is moved through the digestive system by a propulsive action has become mainly waste and water by the time it reaches the large bowel or colon, a 1.5m long tube.
By the time the stool reaches the final section of the colon, it has lost much of the water that was present in the upper part of the digestive system. The stool finally reaches the rectum and—on command from the brain—is then consciously eliminated from the body with a bowel movement through the anal canal.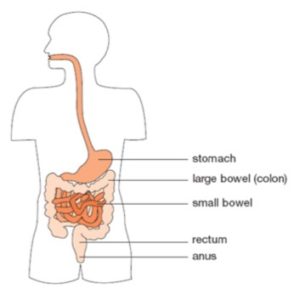
Normal bowel functioning can range from three bowel movements a day to three a week. Despite the widely recommended “one movement a day,” doctors agree that such frequency is not necessary. The medical definition of “infrequent” bowel movements is “less often than once every three days.” Most doctors agree that a movement less than once a week is not adequate. One every two or three days is a preferable minimum. The rectum, the last 10 to 15 cm of the digestive tract, determines when a bowel movement is needed. It remains empty until just before a bowel movement. The filling of the rectum sends messages to the brain via nerves in the rectal wall that a bowel movement is needed.
From the rectum, the stool passes into the anal canal, guarded by ring-shaped, internal and external sphincter muscles. Just prior to being eliminated, the stool is admitted to the anal canal by the internal sphincter muscle, which opens automatically when the rectal wall is stretched by a mass of stool. The external sphincter, on the other hand, is opened by conscious decision of the brain, so that bowel movements can be performed only at appropriate times.
If the contents of the bowel move too fast, not enough water is removed and the stool reaches the rectum in a soft or liquid state known as diarrhoea. If movement of the stool is slow, too much water may be absorbed by the body, making the stool hard and difficult to pass. This condition is constipation. Constipation can prevent any of the stool from being eliminated, or it can result in a partial bowel movement, with part of the waste retained in the bowel or rectum. People may even pass faeces, or stools, at the wrong time or in the wrong place. They may also pass wind without control or totally lose control and soil themselves. This is known as incontinence.
Usual causes
It is important to also know that there can be more usual causes of bowel problems, other than MS. Diarrhoea and constipation can be caused by contaminated food and water, or simply because of a change in an accustomed level of activity. Diarrhoea can also be triggered by a viral, bacterial, or parasitic infection. Continued diarrhoea also stems from food allergies or sensitivity to particular kinds of food, such as highly spiced dishes or dairy products (intolerance to dairy products often can be assisted by drinking lactose-reduced milk or by eating dairy products together with tablets containing lactose-digesting enzymes).
Non-MS related constipation may also be caused by such common medications as calcium supplements or antacids containing aluminium or calcium. Other drugs that may lead to constipation include antidepressants, diuretics, opiates and antipsychotic drugs. Ironically, one of the most common causes of non-MS related constipation is a voluntary habit: delaying bowel movements to save time on busy days, or to avoid the exertion of a trip to the bathroom. Eventually the rectum adapts to the increased bulk of stool and the urge to eliminate subsides. The constipating effects, however, continue and elimination becomes increasingly difficult. For some women, constipation is a premenstrual symptom and, during pregnancy, it may be one way that the colon reacts to a change in the level of sex hormones.
Irritable bowel syndrome
This is also known as spastic colon and is a condition affecting the general population in which constipation and diarrhoea often alternate. It may cause abdominal cramps and wind pains. Irritable bowel syndrome is annoying, but not dangerous and is often associated with stress. Because the symptoms caused by irritable bowel syndrome are similar to those caused by MS, ask your doctor about the possible use and benefits of IBS medications. They may offer some relief.
Constipation and MS
Constipation is the most common bowel complaint of people who have MS. It’s easy to slip into poor dietary habits, physical inactivity and even depression when one lives with MS. All of these can disrupt the digestive system. As explained above, various medications can compound the situation. But there is more to the problem. When MS damages nerve pathways in the brain or spinal cord, a short-circuiting process occurs. This interferes with the signals from the bowel to the brain (indicating the need for a bowel movement), and/or with the responding signals from the brain to the bowel (for maintaining normal functioning). Common MS symptoms such as difficulty in walking and chronic fatigue can lead to slow movement of waste material through the colon. Weakened abdominal muscles can also make the actual process of having a bowel movement more difficult. If the pelvic floor muscles are spastic and unable to relax, normal bowel functioning will be compromised.
Some tend not to have the usual increase in colon activity following meals which propels waste towards the rectum. Finally, some try to solve common bladder problems by reducing their fluid intake. Restricting fluids makes constipation worse. This is so common in MS that the first step to take may be to get medical help for your bladder problems so that adequate fluid intake, so critical to bowel functions, will be possible. A long-term delay is not an option. Besides the obvious discomfort of constipation, complications can develop. Stool that builds up in the rectum can put pressure on part of the urinary system, increasing some bladder problems. A stretched rectum can send messages to the spinal cord that further interrupt bladder function. Constipation aggravates spasticity, making walking more difficult. And constipation can be the root cause of the most distressing bowel symptom, incontinence.
Diarrhoea and MS
In general, diarrhoea is less of a problem for people with MS than constipation. Yet when it occurs, for whatever reasons, it is often compounded by loss of control. Reduced sensation in the rectal area can allow the rectum to stretch beyond its normal range, triggering an unexpected, involuntary relaxation of the external anal sphincter, releasing the loose stool. MS sometimes causes overactive bowel functioning leading to diarrhoea or sphincter abnormalities which can cause incontinence. The condition can be treated with prescription medicines such as Ditropan.
Diarrhoea might indicate a secondary problem, such as gastroenteritis, a parasitic infection or inflammatory bowel disease. It is not wise to treat persistent diarrhoea without a doctor’s advice. Diarrhoea is often managed with a bulk-former, such as Metamucil. When bulk-formers are used to treat diarrhoea instead of constipation, they are taken without any additional fluid. The objective is to take just enough to firm up the stool, but not enough to cause constipation. If bulk-formers do not relieve diarrhoea, your doctor may suggest medications which slow the bowel muscles, such as Kaopectate or Lomotil.
Incontinence
Total loss of bowel control does happen to people with MS. Some people have it as a frequent symptom, others only rarely. If incontinence becomes even an occasional problem, don’t be discouraged. The problem can usually be managed, but it may take some time. Work closely with your doctor and your Regional MS Community Support Staff towards a solution which works for you. A regular schedule of elimination is key. When the bowel becomes used to emptying at specific intervals, accidents at other times are less likely. In addition to drugs, techniques such as biofeedback may help. This can train an individual to be sensitive to subtle signals that the rectum is filling. In the meantime, don’t restrict your life. Protective pants can be used to prevent embarrassing accidents or simply provide peace of mind. An absorbent lining helps protect the skin and a plastic outer lining contains odours and keeps clothing from becoming soiled.
Faecal Impaction
This is a severe form of constipation where a hard mass of stool is lodged in the rectum and cannot be eliminated. This problem requires immediate attention. It can usually be diagnosed through a simple rectal examination, but symptoms may be confusing. Impaction may cause diarrhoea, bowel incontinence, even rectal bleeding from a pressure ulcer of the bowel wall. Your doctor may want you to have a series of tests to rule out the chance of the more serious bowel diseases.
Impaction leads to incontinence when the stool mass presses on the internal sphincter, triggering a relaxation response. The external sphincter, although under voluntary control, is frequently weakened by MS and may not be able to be closed. Watery stool behind the impaction thus leaks out uncontrollably. Diarrhoea as a side effect of constipation is not uncommon in MS. The resulting incontinence may be the first warning a person has that an annoying problem has become a major issue.
Minor bowel symptoms may be easily treated, but persistent or severe symptoms should be evaluated by your doctor. There may be a simple solution, but only your doctor can rule out the more dangerous conditions which a bowel symptom may be signalling. A regular physical checkup normally includes a rectal exam. After the age of 40, men in particular, will want to have periodic examinations of the lower digestive system with a check of the prostate gland at the same time. The methods include a rectal examination or such procedures as a sigmoidoscopy or colonoscopy. These last two tests, in which the bowel is viewed directly with a flexible, lighted tube, are increasingly routine as early diagnostic exams. If you are concerned about any symptoms, at any age, you should consult your health professional for advice.
Whether you are trying to control constipation or diarrhoea or simply want to prevent such problems, following good bowel habits is essential. It is much easier to prevent bowel problems by establishing good habits than to deal with impaction, incontinence or laxative dependency later on. If your bowel movements are becoming less frequent, take action. You may be able to prevent worsening constipation problems by following the good bowel habits outlined here. Stool that is retained for long periods tends to stretch the bowel, reducing its ability to push waste from the body. The stool also becomes harder with time, making elimination more and more difficult.
Drink enough fluids
Each day, drink eight to ten cups whether you are thirsty or not. Water, juices, coffee and other beverages all count. But common MS-related bladder problems can easily complicate this part of good bowel habits. It is hard to drink adequate fluid if one is wakened up at night because of the need to urinate or contending with urinary urgency, frequency, leaking or loss of bladder control. These are ‘red-flag’ problems for people with MS. But bladder problems can be controlled if the underlying cause is identified. See your doctor—treat bladder symptoms first.
Put fibre in your diet
Fibre is plant material which holds water and is resistant to digestion. It is found in wholegrain breads and cereals as well as in raw fruits and vegetables. Fibre helps keep the stool moving by adding bulk to the contents of the bowel and by softening the stool with water. Incorporate high-fibre foods into your diet gradually to lessen the chances of gas, bloating or diarrhoea. Getting enough fibre in your daily diet may require more than eating fruits and vegetables. It may be helpful to eat a daily bowlful of bran cereal plus up to four slices of a bran-containing bread each day. If you have limited mobility, you may need as much as 30 grams of fibre a day to control constipation. Still, each person’s fibre needs are different. Add fibre slowly. Diarrhoea or too frequent bowel movements can result from a diet to high in fibre. If you find you cannot tolerate a high-fibre diet, your doctor may prescribe high fibre compounds such as psyllium hydrophilic muciloid or calcium polycarbophil.
Regular physical activity
Walking, swimming and even wheelchair exercises help. With age, a person’s activity level decreases. Although the type of activity may need to be changed, some regular exercise is important at any age or any stage of disability.
Establish a regular time of day for a bowel movement
The best time of day is about half an hour after eating, when the emptying reflex is strongest. It is strongest of all after breakfast. Set aside 20 to 30 minutes for this routine. Because MS can decrease sensation in the rectal area, you may not always feel the urge to eliminate. Stick to the routine of a regular time each day for a bowel movement, whether or not you have the urge. It may also help to decrease the angle between the rectum and the anus, which can be done by reducing the distance from the toilet seat to the floor to between 30 and 38 cm. Many people, however, with mobility problems raise the seat for ease of use. A footstool can create the same desired body angle, by raising your feet once you are seated. Avoid unnecessary stress, Your emotions affect your physical state, including the functioning of your bowel. Take your time. Use relaxation techniques. Remember that a successful bowel schedule often takes time to become established. Depression has been known to cause constipation. The constipation can upset you further, starting an unnecessary cycle of worsening conditions. If your emotions are troubling you, talk to your doctor and/or your Regional MS Community Support Staff or read our booklet ‘MS and Your Emotions’ available in this series.
If the steps outlined above fail to address your constipation problems, your doctor will probably suggest the following remedies.
Stool softeners
These products should be used sparingly, however, as some of them may increase the side effects of other drugs, especially those taken at the same time. The use of mineral oil is not advised, because it can reduce the absorption of fat-soluble vitamins and is hazardous to inhale.
Bulk supplements
Natural fibre supplements include Metamucil, which if taken daily with one or two glasses of water, help fill and moisturise the gastrointestinal tract. These bulk-forming agents are generally safe to take for long periods.
Mild oral laxatives
Milk of Magnesia or epsom salts are all osmotic agents. This means they promote secretion of water into the colon and they are reasonably safe. Another mild laxative is Senokot. This is an example of a stimulant laxative, which provides a chemical irritant to the bowel, thus stimulating the passages of stool. Harsh laxatives, such as Brooklax, Dulcolax or castor oil can be highly habit-forming and are rarely recommended for MS bowel problems. The gentler laxatives usually induce bowel movements within eight to 12 hours.
Suppositories
If oral laxatives fail to provide relief, you may be told to try a glycerine suppository half an hour before attempting a bowel movement. This practice may be necessary for several weeks in order to establish a regular bowel routine. For some people, suppositories are needed on a permanent basis. Dulcolax suppositories stimulate a strong, wave-like movement of rectal muscles, but they are much more habit-forming than are suppositories containing glycerine.
Enemas
Enemas should be used sparingly because the body may come to depend on them. They may be recommended as part of a therapy that includes stool-softeners, bulk supplements and mild oral laxatives.
Manual stimulation
You can sometimes promote elimination by gently massaging the abdomen in a clockwise direction, or by inserting a finger in the rectum and rotating it gently. It is advisable to wear a plastic finger covering or plastic glove. Note: In using any of these techniques to control constipation, remember that they all take time—often several weeks before it is clear how well they are working. The digestive rhythm can be modified only gradually.
As with many other kinds of medical problems, it’s easier to treat the bowel and related parts of the digestive system with good preventive habits than to wait until problems develop.
Remember: Treat bladder problems first, eat plenty of fruits, vegetables, fibre and fluids every day. Exercise daily and use the toilet half-an-hour after breakfast every day.
Dealing with impaction, incontinence and a chronic dependence on laxatives is much more difficult than preventing those situations or treating their precursors. Try the mildest therapies first, as stronger measures are more likely to have side effects.
Many MS symptoms, such as bladder problems, spasticity, weakness, immobility and demyelination which interfere with communication between your bowel and your brain can lead to bowel complications. If problems persist or worsen, ask your doctor for a referral to a gastroenterologist, who specialises in bowel and other digestive problems.
For more information please view our MSNZ Information Series booklet: Multiple Sclerosis and your bladder and bowel